Are Fallen Arches Flat Feet?
Overview

A normal foot should arch so the middle of the foot does not touch the ground when the patient stands up. If it does touch, the patient has a flat foot or fallen arch. Flat feet are normal for young children. Their arches should develop by adulthood, but sometimes they fail to develop. Some people with flat feet have pain in the heel or arch, but others do not.
Causes
Flat feet are often a congenital problem which has no specific cause. They can however occur after an injury, especially conditions such as Tibialis Posterior Syndrome or more traumatic injuries such as fractures or mid-tarsal joint sprains. The other thing to look out for is Overpronation. Often this is confused with having flat feet (or a fallen arch) although it is not technically the same thing. If an individual does not have flat feet but does overpronate then the arch of their foot appears to be normal when standing. However, when they walk the arch collapses and the foot rolls in excessively. This is more difficult to spot than flat feet. It is estimated that between 60 and 80% of the population overpronate!
Symptoms
Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area. Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time. Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot. The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
You can always give yourself the ?wet test? described above to see whether you have flat feet. Most people who do not notice their flat feet or have no pain associated with them do not think to see a foot doctor. Flat feet can lead to additional problems such as stiffness or pain, however, especially if the condition appears out of nowhere. If you think you may have flat feet, you should seek medical attention to ensure there are no additional issues to worry about. Your doctor will be able to diagnose you with a number of tests. For example, he or she may have you walk around, stand still, or stand on your tiptoes while you are being examined. Your doctor may also examine your foot?s shape and functionality. It?s important to let your foot doctor know about your medical and family history. In some cases, your doctor may order imaging tests such as x-rays or an MRI (magnetic resonance imaging) to determine a cause of your flat foot. If tarsal coalition is suspected in children, a CT scan is often ordered.
pes planus treatment
Non Surgical Treatment
Flexible flat feet that are painless do not require treatment. If you have pain due to flexible flat feet, an orthotic (arch-supporting insert in the shoe) can bring relief. With the increased interest in running, many shoe stores carry shoes for normal feet and pronated feet. The shoes designed for pronated feet make long distance running easier and less tiring because they correct for the abnormality. Rigid or painful flat feet require evaluation by a health care provider. The treatment depends on the cause of the flat feet. For tarsal coalition, treatment starts with rest and possibly a cast. If this fails to improve the pain, surgery may be necessary. For problems with the posterior tibial tendon, treatment may start with rest, anti-inflammatory medications, and shoe inserts or ankle braces. In more advanced cases, surgery may be needed to clean or repair the tendon, or fuse some of the joints of the foot into a corrected position. Flat feet in older adults can be treated with pain relievers, orthotics, and sometimes surgery.
Surgical Treatment

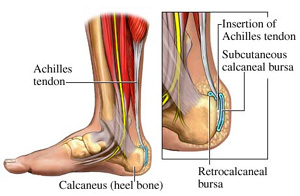
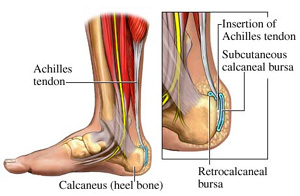
Since there are many different causes of flatfoot, the types of flatfoot reconstruction surgery are best categorized by the conditions. Posterior tibial tendon dysfunction. In this condition, the tendon connecting the calf muscle to the inner foot is torn or inflamed. Once the tendon is damaged it no longer can serve its main function of supporting the arch of the foot. Flatfoot is the main result of this type of condition and can be treated by the following flatfoot reconstruction surgeries. Lengthening of the Achilles tendon. Otherwise known as gastrocnemius recession, this procedure is used to lengthen the calf muscles in the leg. This surgery treats flatfoot and prevents it from returning in the future. This procedure is often combined with other surgeries to correct posterior tibial tendon dysfunction. Cleaning the tendon. Also known as tenosynovectomy, this procedure is used in the earlier and less severe stages of posterior tibial tendon dysfunction. It is performed before the arch collapses and while the tendon is only mildly affected. The inflamed tissue is cleaned away and removed from the remaining healthy tendon. Tendon transfer. This procedure is done to correct flatfoot and reform the lost arch in the foot. During the procedure, the diseased tendon is removed and replaced by tendon from another area of the foot. If the tendon is only partially damaged, the inflamed part is cleaned and removed then attached to a new tendon. Cutting and shifting bones. Also called an osteotomy, this procedure consists of cutting and reconstructing bones in the foot to reconstruct the arch. The heel bone and the midfoot are most likely reshaped to achieve this desired result. A bone graft may be used to fuse the bones or to lengthen the outside of the foot. Temporary instrumentation such as screws and plates can also be used to hold the bones together while they heal.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.

A normal foot should arch so the middle of the foot does not touch the ground when the patient stands up. If it does touch, the patient has a flat foot or fallen arch. Flat feet are normal for young children. Their arches should develop by adulthood, but sometimes they fail to develop. Some people with flat feet have pain in the heel or arch, but others do not.
Causes
Flat feet are often a congenital problem which has no specific cause. They can however occur after an injury, especially conditions such as Tibialis Posterior Syndrome or more traumatic injuries such as fractures or mid-tarsal joint sprains. The other thing to look out for is Overpronation. Often this is confused with having flat feet (or a fallen arch) although it is not technically the same thing. If an individual does not have flat feet but does overpronate then the arch of their foot appears to be normal when standing. However, when they walk the arch collapses and the foot rolls in excessively. This is more difficult to spot than flat feet. It is estimated that between 60 and 80% of the population overpronate!
Symptoms
Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area. Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time. Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot. The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
You can always give yourself the ?wet test? described above to see whether you have flat feet. Most people who do not notice their flat feet or have no pain associated with them do not think to see a foot doctor. Flat feet can lead to additional problems such as stiffness or pain, however, especially if the condition appears out of nowhere. If you think you may have flat feet, you should seek medical attention to ensure there are no additional issues to worry about. Your doctor will be able to diagnose you with a number of tests. For example, he or she may have you walk around, stand still, or stand on your tiptoes while you are being examined. Your doctor may also examine your foot?s shape and functionality. It?s important to let your foot doctor know about your medical and family history. In some cases, your doctor may order imaging tests such as x-rays or an MRI (magnetic resonance imaging) to determine a cause of your flat foot. If tarsal coalition is suspected in children, a CT scan is often ordered.
pes planus treatment
Non Surgical Treatment
Flexible flat feet that are painless do not require treatment. If you have pain due to flexible flat feet, an orthotic (arch-supporting insert in the shoe) can bring relief. With the increased interest in running, many shoe stores carry shoes for normal feet and pronated feet. The shoes designed for pronated feet make long distance running easier and less tiring because they correct for the abnormality. Rigid or painful flat feet require evaluation by a health care provider. The treatment depends on the cause of the flat feet. For tarsal coalition, treatment starts with rest and possibly a cast. If this fails to improve the pain, surgery may be necessary. For problems with the posterior tibial tendon, treatment may start with rest, anti-inflammatory medications, and shoe inserts or ankle braces. In more advanced cases, surgery may be needed to clean or repair the tendon, or fuse some of the joints of the foot into a corrected position. Flat feet in older adults can be treated with pain relievers, orthotics, and sometimes surgery.
Surgical Treatment

Since there are many different causes of flatfoot, the types of flatfoot reconstruction surgery are best categorized by the conditions. Posterior tibial tendon dysfunction. In this condition, the tendon connecting the calf muscle to the inner foot is torn or inflamed. Once the tendon is damaged it no longer can serve its main function of supporting the arch of the foot. Flatfoot is the main result of this type of condition and can be treated by the following flatfoot reconstruction surgeries. Lengthening of the Achilles tendon. Otherwise known as gastrocnemius recession, this procedure is used to lengthen the calf muscles in the leg. This surgery treats flatfoot and prevents it from returning in the future. This procedure is often combined with other surgeries to correct posterior tibial tendon dysfunction. Cleaning the tendon. Also known as tenosynovectomy, this procedure is used in the earlier and less severe stages of posterior tibial tendon dysfunction. It is performed before the arch collapses and while the tendon is only mildly affected. The inflamed tissue is cleaned away and removed from the remaining healthy tendon. Tendon transfer. This procedure is done to correct flatfoot and reform the lost arch in the foot. During the procedure, the diseased tendon is removed and replaced by tendon from another area of the foot. If the tendon is only partially damaged, the inflamed part is cleaned and removed then attached to a new tendon. Cutting and shifting bones. Also called an osteotomy, this procedure consists of cutting and reconstructing bones in the foot to reconstruct the arch. The heel bone and the midfoot are most likely reshaped to achieve this desired result. A bone graft may be used to fuse the bones or to lengthen the outside of the foot. Temporary instrumentation such as screws and plates can also be used to hold the bones together while they heal.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Heel Discomfort All The Things You Should Understand Heel Discomfort
Overview

The most common cause of heel pain is inflammation due to injury of the soft tissue around your heel. The plantar fascia is the area of your foot most likely to be inflamed, which results in plantar fasciitis. With plantar fasciitis, you experience a sharp burning or stabbing sensation upon arising after walking or standing for prolonged periods. Your first steps each morning probably hurt, too. Heel pain is occasionally caused by excessive pounding on the heels. This is more common in the elderly and overweight individuals whose heel fat pads no longer function properly. Watch for a bruising sensation under the heel when standing and walking. If you think this is your issue, an insert with an artificial fat pad might help alleviate your discomfort. Heel pain is by far the most common foot complaint. There are many medical conditions that are associated with heel pain, including gout and other forms of arthritis.
Causes
Heel pain is often the result of the plantar fascia being overstretched or overused. Risk factors include. Obesity or sudden weight gain. Long distance running. Tight Achilles tendons. Shoes with poor arch support or soft soles. Foot arch problems (both high arches and flat feet).
Symptoms
Symptoms of plantar fasciitis vary, but the classic symptom is pain after rest--when you first get out of bed in the morning, or when you get up after sitting down for a while during the day. The pain usually diminishes after a few minutes of walking, sometimes even disappearing, but the pain is commonly felt again the longer you're on the foot. Fasciitis can be aggravated by shoes that lack appropriate support, especially in the arch area, and by the chronic irritation of long-periods of standing, especially on concrete, by being overweight. It doesn't help that fascia doesn't heal particularly quickly because it has relatively poor circulation (which is why it's white in colour).
Diagnosis
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
Morning Wall Stretch. Stand barefoot in front of wall, as shown. Press into wall with both hands and lean forward, feeling stretch along back of left leg and heel. Hold for 30 seconds; switch sides and repeat. Freeze and Roll. Freeze a small water bottle. Cover it with a towel and place arch of your foot on top of it. Slowly roll bottle beneath arch of foot for about 5 minutes at a time. Switch sides and repeat. Rub It Out. Use both thumbs to apply deep pressure along arch of the feet, heel, and calf muscles, moving slowly and evenly. Continue for 1 minute. Switch sides and repeat. If you foot pain isn't improving or worsens after 2 weeks, a podiatrist or othopedist can prescribe additional therapies to alleviate discomfort and prevent recurrence.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
heelsncleavage
Prevention
You can help to prevent heel pain by maintaining a healthy weight, by warming up before participating in sports and by wearing shoes that support the arch of the foot and cushion the heel. If you are prone to plantar fasciitis, exercises that stretch the Achilles tendon (heel cord) and plantar fascia may help to prevent the area from being injured again. You also can massage the soles of your feet with ice after stressful athletic activities. Sometimes, the only interventions needed are a brief period of rest and new walking or running shoes.

The most common cause of heel pain is inflammation due to injury of the soft tissue around your heel. The plantar fascia is the area of your foot most likely to be inflamed, which results in plantar fasciitis. With plantar fasciitis, you experience a sharp burning or stabbing sensation upon arising after walking or standing for prolonged periods. Your first steps each morning probably hurt, too. Heel pain is occasionally caused by excessive pounding on the heels. This is more common in the elderly and overweight individuals whose heel fat pads no longer function properly. Watch for a bruising sensation under the heel when standing and walking. If you think this is your issue, an insert with an artificial fat pad might help alleviate your discomfort. Heel pain is by far the most common foot complaint. There are many medical conditions that are associated with heel pain, including gout and other forms of arthritis.
Causes
Heel pain is often the result of the plantar fascia being overstretched or overused. Risk factors include. Obesity or sudden weight gain. Long distance running. Tight Achilles tendons. Shoes with poor arch support or soft soles. Foot arch problems (both high arches and flat feet).
Symptoms
Symptoms of plantar fasciitis vary, but the classic symptom is pain after rest--when you first get out of bed in the morning, or when you get up after sitting down for a while during the day. The pain usually diminishes after a few minutes of walking, sometimes even disappearing, but the pain is commonly felt again the longer you're on the foot. Fasciitis can be aggravated by shoes that lack appropriate support, especially in the arch area, and by the chronic irritation of long-periods of standing, especially on concrete, by being overweight. It doesn't help that fascia doesn't heal particularly quickly because it has relatively poor circulation (which is why it's white in colour).
Diagnosis
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
Morning Wall Stretch. Stand barefoot in front of wall, as shown. Press into wall with both hands and lean forward, feeling stretch along back of left leg and heel. Hold for 30 seconds; switch sides and repeat. Freeze and Roll. Freeze a small water bottle. Cover it with a towel and place arch of your foot on top of it. Slowly roll bottle beneath arch of foot for about 5 minutes at a time. Switch sides and repeat. Rub It Out. Use both thumbs to apply deep pressure along arch of the feet, heel, and calf muscles, moving slowly and evenly. Continue for 1 minute. Switch sides and repeat. If you foot pain isn't improving or worsens after 2 weeks, a podiatrist or othopedist can prescribe additional therapies to alleviate discomfort and prevent recurrence.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
heelsncleavage
Prevention
You can help to prevent heel pain by maintaining a healthy weight, by warming up before participating in sports and by wearing shoes that support the arch of the foot and cushion the heel. If you are prone to plantar fasciitis, exercises that stretch the Achilles tendon (heel cord) and plantar fascia may help to prevent the area from being injured again. You also can massage the soles of your feet with ice after stressful athletic activities. Sometimes, the only interventions needed are a brief period of rest and new walking or running shoes.
Leg Length Discrepancy
Overview
Leg length discrepancy is an orthopaedic problem that usually appears in childhood, in which one's two legs are of unequal lengths. Often abbreviated as ?LLD,' leg length discrepancy may be caused by or associated with a number of other orthopaedic or medical conditions, but is generally treated in a similar fashion, regardless of cause and depending on severity. Leg length discrepancy is sometimes divided up into 'true LLD' and 'functional LLD.' Functional LLD occurs when the legs are actually equal in length, but some other condition, such as pelvic obliquity (a tilt in the position of the pelvis), creates the appearance of legs of different lengths.
Causes
LLDs are very common. Sometimes the cause isn?t known. But the known causes of LLD in children include, injury or infection that slows growth of one leg bone. Injury to the growth plate (a soft part of a long bone that allows the bone to grow). Growth plate injury can slow bone growth in that leg. Fracture to a leg bone that causes overgrowth of the bone as it heals. A congenital (present at birth) problem (one whole side of the child?s body may be larger than the other side). Conditions that affect muscles and nerves, such as polio.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
A doctor will generally take a detailed medical history of both the patient and family, including asking about recent injuries or illnesses. He or she will carefully examine the patient, observing how he or she moves and stands. If necessary, an orthopedic surgeon will order X-ray, bone age determinations and computed tomography (CT) scans or magnetic resonance imaging (MRI).
Non Surgical Treatment
A properly made foot orthotic can go a long way in substituting additional millimeters or centimeter on the deficient side. Additional full length inserts are added to the shorter side bringing the runner closer to symmetrical. Heel lifts do not work in runners because when you run you may land on your heel but the rest of the time you are on your forefoot then your toes pushing off. The right custom-made, biomechanical orthotic can address the underlying cause of your pain. Abnormal joint position, overpronation or foot rigidity can be addressed and the biomechanics normalized. San Diego Running Institute orthotics are custom molded to your foot and are designed with your specific body weight, leg length discrepancy, and activity in mind. The restoration of correct mechanical function takes the abnormal stress from the uneven side and allows the body to heal naturally.

height increase exercises
Surgical Treatment
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.
Leg length discrepancy is an orthopaedic problem that usually appears in childhood, in which one's two legs are of unequal lengths. Often abbreviated as ?LLD,' leg length discrepancy may be caused by or associated with a number of other orthopaedic or medical conditions, but is generally treated in a similar fashion, regardless of cause and depending on severity. Leg length discrepancy is sometimes divided up into 'true LLD' and 'functional LLD.' Functional LLD occurs when the legs are actually equal in length, but some other condition, such as pelvic obliquity (a tilt in the position of the pelvis), creates the appearance of legs of different lengths.

Causes
LLDs are very common. Sometimes the cause isn?t known. But the known causes of LLD in children include, injury or infection that slows growth of one leg bone. Injury to the growth plate (a soft part of a long bone that allows the bone to grow). Growth plate injury can slow bone growth in that leg. Fracture to a leg bone that causes overgrowth of the bone as it heals. A congenital (present at birth) problem (one whole side of the child?s body may be larger than the other side). Conditions that affect muscles and nerves, such as polio.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
A doctor will generally take a detailed medical history of both the patient and family, including asking about recent injuries or illnesses. He or she will carefully examine the patient, observing how he or she moves and stands. If necessary, an orthopedic surgeon will order X-ray, bone age determinations and computed tomography (CT) scans or magnetic resonance imaging (MRI).
Non Surgical Treatment
A properly made foot orthotic can go a long way in substituting additional millimeters or centimeter on the deficient side. Additional full length inserts are added to the shorter side bringing the runner closer to symmetrical. Heel lifts do not work in runners because when you run you may land on your heel but the rest of the time you are on your forefoot then your toes pushing off. The right custom-made, biomechanical orthotic can address the underlying cause of your pain. Abnormal joint position, overpronation or foot rigidity can be addressed and the biomechanics normalized. San Diego Running Institute orthotics are custom molded to your foot and are designed with your specific body weight, leg length discrepancy, and activity in mind. The restoration of correct mechanical function takes the abnormal stress from the uneven side and allows the body to heal naturally.

height increase exercises
Surgical Treatment
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.
What Causes Mortons Neuroma
Overview
 Morton?s neuroma is inflammation, thickening, or enlargement of the nerve between the bones of the toes (metatarsal bones). The condition is also called intermetatarsal neuroma. The thickening is usually found between bones of the third and fourth toes of the foot, but sometimes it may develop between the second and third toes. It occurs when the medial plantar nerve near the bones of those toes becomes compressed or irritated, possibly because the metatarsal bones press against the nerve in the narrow gap between the toes. If left untreated, Morton?s neuroma can cause a sharp, burning, or shooting pain that often gets worse over time. The pain becomes worse when a person walks or stands on the ball of the foot. Sometimes the pain reaches the toes next to the neuroma and a sensation of tingling or numbness is felt.
Morton?s neuroma is inflammation, thickening, or enlargement of the nerve between the bones of the toes (metatarsal bones). The condition is also called intermetatarsal neuroma. The thickening is usually found between bones of the third and fourth toes of the foot, but sometimes it may develop between the second and third toes. It occurs when the medial plantar nerve near the bones of those toes becomes compressed or irritated, possibly because the metatarsal bones press against the nerve in the narrow gap between the toes. If left untreated, Morton?s neuroma can cause a sharp, burning, or shooting pain that often gets worse over time. The pain becomes worse when a person walks or stands on the ball of the foot. Sometimes the pain reaches the toes next to the neuroma and a sensation of tingling or numbness is felt.
Causes
In many cases, a neuroma may develop as a result of excessive loading on the front of the foot. Sometimes, a patient?s anatomic alignment in the forefoot contributes to the overload. There may be some cases where the neuroma develops spontaneously, for no obvious reason. However, once the nerve is irritated, pressure from walking, and from the adjacent bony prominences (metatarsal heads), as well as from the intermetatarsal ligament that binds the heads together, all may contribute to persistent pain. Repetitive pressure on the nerve causes localized injury with resulting scarring and fibrosis of the nerve. This leads to symptoms in the distribution of the nerve.
Symptoms
Typically, there's no outward sign of this condition, such as a lump. Instead, you may experience the following symptoms. A feeling as if you're standing on a pebble in your shoe. A burning pain in the ball of your foot that may radiate into your toes. Tingling or numbness in your toes. It's best not to ignore any foot pain that lasts longer than a few days. See your doctor if you experience a burning pain in the ball of your foot that's not improving, despite changing your footwear and modifying activities that may cause stress to your foot.
Diagnosis
The exact cause of Mortons neuroma can often vary between patients. An accurate diagnosis must be carefully made by the podiatrist through thorough history taking and direct questioning to ensure all possible causes are addressed. The podiatrist will also gather further information about the cause through a hands on assessment where they will try to reproduce your symptoms. A biomechanical and gait analysis will also be performed to assess whether poor foot alignment and function has contributed to your neuroma.
Non Surgical Treatment
Treatment for Morton's neuroma may depend on several factors, including the severity of symptoms and how long they have been present. The earlier on the condition is diagnosed, the less likely surgery is required. Doctors will usually recommend self-help measures first. These may include resting the foot, massaging the foot and affected toes. Using an ice pack on the affected area (skin should not be directly exposed to ice, the ice should be in a container or wrapped in something) Changing footwear, wearing wide-toed shoes, or flat (non high-heeled) shoes. Trying arch supports (orthotic devices). A type of padding that supports the arch of the foot, removing pressure from the nerve. The doctor may recommend a custom-made, individually designed shoe-insert, molded to fit the contours of the patient's foot. There are several OTC (over the counter, non-prescription) metatarsal pads or bars available which can be placed over the neuroma. Taking over-the-counter, non-prescription painkilling medications. Modifying activities, avoiding activities which put repetitive pressure on the neuroma until the condition improves. Bodyweight management,if the patient is obese the doctor may advise him/her to lose weight. A significant number of obese patients with foot problems, such as flat feet, who successfully lose weight experience considerable improvement of symptoms.
Surgical Treatment
Surgery for neuroma most often involves removing affected nerve in the ball of the foot. An incision is made on the top of the foot and the nerve is carefully removed. Surgeon must remove the nerve far enough back so that the nerve doesn?t continue to become impinged at the ball of the foot. Alternatitvely, another type of surgery involves releasing a tight ligament that encases the nerve. Recovery after Morton?s neuroma (neurectomy) surgery is generally quick. Typically patients are walking on the operated foot in a post-surgical shoe for 2 - 4 weeks, depending on healing. Return to shoes is 2-6 weeks after the surgery. Factors that may prolong healing are age, smoking, poor nutritional status, and some medical problems.
 Morton?s neuroma is inflammation, thickening, or enlargement of the nerve between the bones of the toes (metatarsal bones). The condition is also called intermetatarsal neuroma. The thickening is usually found between bones of the third and fourth toes of the foot, but sometimes it may develop between the second and third toes. It occurs when the medial plantar nerve near the bones of those toes becomes compressed or irritated, possibly because the metatarsal bones press against the nerve in the narrow gap between the toes. If left untreated, Morton?s neuroma can cause a sharp, burning, or shooting pain that often gets worse over time. The pain becomes worse when a person walks or stands on the ball of the foot. Sometimes the pain reaches the toes next to the neuroma and a sensation of tingling or numbness is felt.
Morton?s neuroma is inflammation, thickening, or enlargement of the nerve between the bones of the toes (metatarsal bones). The condition is also called intermetatarsal neuroma. The thickening is usually found between bones of the third and fourth toes of the foot, but sometimes it may develop between the second and third toes. It occurs when the medial plantar nerve near the bones of those toes becomes compressed or irritated, possibly because the metatarsal bones press against the nerve in the narrow gap between the toes. If left untreated, Morton?s neuroma can cause a sharp, burning, or shooting pain that often gets worse over time. The pain becomes worse when a person walks or stands on the ball of the foot. Sometimes the pain reaches the toes next to the neuroma and a sensation of tingling or numbness is felt.Causes
In many cases, a neuroma may develop as a result of excessive loading on the front of the foot. Sometimes, a patient?s anatomic alignment in the forefoot contributes to the overload. There may be some cases where the neuroma develops spontaneously, for no obvious reason. However, once the nerve is irritated, pressure from walking, and from the adjacent bony prominences (metatarsal heads), as well as from the intermetatarsal ligament that binds the heads together, all may contribute to persistent pain. Repetitive pressure on the nerve causes localized injury with resulting scarring and fibrosis of the nerve. This leads to symptoms in the distribution of the nerve.
Symptoms
Typically, there's no outward sign of this condition, such as a lump. Instead, you may experience the following symptoms. A feeling as if you're standing on a pebble in your shoe. A burning pain in the ball of your foot that may radiate into your toes. Tingling or numbness in your toes. It's best not to ignore any foot pain that lasts longer than a few days. See your doctor if you experience a burning pain in the ball of your foot that's not improving, despite changing your footwear and modifying activities that may cause stress to your foot.
Diagnosis
The exact cause of Mortons neuroma can often vary between patients. An accurate diagnosis must be carefully made by the podiatrist through thorough history taking and direct questioning to ensure all possible causes are addressed. The podiatrist will also gather further information about the cause through a hands on assessment where they will try to reproduce your symptoms. A biomechanical and gait analysis will also be performed to assess whether poor foot alignment and function has contributed to your neuroma.
Non Surgical Treatment
Treatment for Morton's neuroma may depend on several factors, including the severity of symptoms and how long they have been present. The earlier on the condition is diagnosed, the less likely surgery is required. Doctors will usually recommend self-help measures first. These may include resting the foot, massaging the foot and affected toes. Using an ice pack on the affected area (skin should not be directly exposed to ice, the ice should be in a container or wrapped in something) Changing footwear, wearing wide-toed shoes, or flat (non high-heeled) shoes. Trying arch supports (orthotic devices). A type of padding that supports the arch of the foot, removing pressure from the nerve. The doctor may recommend a custom-made, individually designed shoe-insert, molded to fit the contours of the patient's foot. There are several OTC (over the counter, non-prescription) metatarsal pads or bars available which can be placed over the neuroma. Taking over-the-counter, non-prescription painkilling medications. Modifying activities, avoiding activities which put repetitive pressure on the neuroma until the condition improves. Bodyweight management,if the patient is obese the doctor may advise him/her to lose weight. A significant number of obese patients with foot problems, such as flat feet, who successfully lose weight experience considerable improvement of symptoms.

Surgical Treatment
Surgery for neuroma most often involves removing affected nerve in the ball of the foot. An incision is made on the top of the foot and the nerve is carefully removed. Surgeon must remove the nerve far enough back so that the nerve doesn?t continue to become impinged at the ball of the foot. Alternatitvely, another type of surgery involves releasing a tight ligament that encases the nerve. Recovery after Morton?s neuroma (neurectomy) surgery is generally quick. Typically patients are walking on the operated foot in a post-surgical shoe for 2 - 4 weeks, depending on healing. Return to shoes is 2-6 weeks after the surgery. Factors that may prolong healing are age, smoking, poor nutritional status, and some medical problems.
Shoe Lifts For Leg Length Discrepancy
There are actually not one but two different kinds of leg length discrepancies, congenital and acquired. Congenital means that you are born with it. One leg is structurally shorter in comparison to the other. As a result of developmental stages of aging, the human brain senses the step pattern and recognizes some variation. Our bodies usually adapts by tilting one shoulder to the "short" side. A difference of less than a quarter inch isn't really abnormal, require Shoe Lifts to compensate and ordinarily does not have a profound effect over a lifetime.

Leg length inequality goes mainly undiagnosed on a daily basis, yet this condition is easily remedied, and can eliminate a number of cases of back pain.
Treatment for leg length inequality commonly involves Shoe Lifts. These are typically cost-effective, typically costing less than twenty dollars, compared to a custom orthotic of $200 and up. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Upper back pain is easily the most widespread ailment impacting people today. Over 80 million people suffer from back pain at some stage in their life. It is a problem which costs employers millions year after year as a result of lost time and output. Innovative and superior treatment solutions are continually sought after in the hope of reducing the economic impact this condition causes.

People from all corners of the world suffer the pain of foot ache as a result of leg length discrepancy. In these types of cases Shoe Lifts might be of immense help. The lifts are capable of relieving any discomfort in the feet. Shoe Lifts are recommended by many skilled orthopaedic physicians.
In order to support the body in a nicely balanced manner, your feet have a very important part to play. Irrespective of that, it is often the most overlooked area in the body. Many people have flat-feet meaning there is unequal force placed on the feet. This will cause other areas of the body such as knees, ankles and backs to be affected too. Shoe Lifts guarantee that proper posture and balance are restored.

Leg length inequality goes mainly undiagnosed on a daily basis, yet this condition is easily remedied, and can eliminate a number of cases of back pain.
Treatment for leg length inequality commonly involves Shoe Lifts. These are typically cost-effective, typically costing less than twenty dollars, compared to a custom orthotic of $200 and up. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Upper back pain is easily the most widespread ailment impacting people today. Over 80 million people suffer from back pain at some stage in their life. It is a problem which costs employers millions year after year as a result of lost time and output. Innovative and superior treatment solutions are continually sought after in the hope of reducing the economic impact this condition causes.

People from all corners of the world suffer the pain of foot ache as a result of leg length discrepancy. In these types of cases Shoe Lifts might be of immense help. The lifts are capable of relieving any discomfort in the feet. Shoe Lifts are recommended by many skilled orthopaedic physicians.
In order to support the body in a nicely balanced manner, your feet have a very important part to play. Irrespective of that, it is often the most overlooked area in the body. Many people have flat-feet meaning there is unequal force placed on the feet. This will cause other areas of the body such as knees, ankles and backs to be affected too. Shoe Lifts guarantee that proper posture and balance are restored.
Leg Length Discrepancy And Shoe Lifts
There are two different types of leg length discrepancies, congenital and acquired. Congenital means that you are born with it. One leg is structurally shorter than the other. Through developmental periods of aging, the brain picks up on the step pattern and identifies some variance. Our bodies typically adapts by dipping one shoulder to the "short" side. A difference of under a quarter inch isn't blatantly irregular, demand Shoe Lifts to compensate and in most cases does not have a profound effect over a lifetime.

Leg length inequality goes largely undiagnosed on a daily basis, however this problem is very easily solved, and can reduce a number of incidents of chronic back pain.
Therapy for leg length inequality typically involves Shoe Lifts. These are low-priced, often costing less than twenty dollars, compared to a custom orthotic of $200 and up. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is easily the most common condition impacting men and women today. Around 80 million people experience back pain at some stage in their life. It's a problem which costs employers huge amounts of money yearly due to lost time and production. Innovative and more effective treatment solutions are constantly sought after in the hope of reducing the economical impact this issue causes.

People from all corners of the world experience foot ache as a result of leg length discrepancy. In these situations Shoe Lifts might be of beneficial. The lifts are capable of easing any discomfort in the feet. Shoe Lifts are recommended by many experienced orthopaedic orthopedists.
In order to support the human body in a well-balanced fashion, the feet have a very important function to play. In spite of that, it is sometimes the most overlooked zone in the human body. Many people have flat-feet meaning there may be unequal force placed on the feet. This causes other body parts such as knees, ankles and backs to be impacted too. Shoe Lifts make sure that proper posture and balance are restored.

Leg length inequality goes largely undiagnosed on a daily basis, however this problem is very easily solved, and can reduce a number of incidents of chronic back pain.
Therapy for leg length inequality typically involves Shoe Lifts. These are low-priced, often costing less than twenty dollars, compared to a custom orthotic of $200 and up. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is easily the most common condition impacting men and women today. Around 80 million people experience back pain at some stage in their life. It's a problem which costs employers huge amounts of money yearly due to lost time and production. Innovative and more effective treatment solutions are constantly sought after in the hope of reducing the economical impact this issue causes.

People from all corners of the world experience foot ache as a result of leg length discrepancy. In these situations Shoe Lifts might be of beneficial. The lifts are capable of easing any discomfort in the feet. Shoe Lifts are recommended by many experienced orthopaedic orthopedists.
In order to support the human body in a well-balanced fashion, the feet have a very important function to play. In spite of that, it is sometimes the most overlooked zone in the human body. Many people have flat-feet meaning there may be unequal force placed on the feet. This causes other body parts such as knees, ankles and backs to be impacted too. Shoe Lifts make sure that proper posture and balance are restored.
What Can Lead To Heel Spur

Overview
There are approximately 75 different causes of heel pain. At least 80% of all heel pain is due to heel spurs. A heel spur contains calcium, but cannot truly be called a calcium deposit. Bone spurs, whether they are on the heel or on any other bone of the body, are true bone -- they are true enlargements of the bone and may be sharp and pointed, or round and knobby. Since bone spurs are true bone, they contain calcium just like regular bones, but are not pure calcium deposits.
Causes
The cause of heel spurs is excessive strain placed on the plantar fascia over a long period of time, as a result of different factors. These factors include incorrect gait, being overweight, ageing or being in a job that requires a lot of standing on hard floors. It is usually a combination of any of these factors that will bring on the development of heel spurs.

Symptoms
The Heel Spur itself is not thought to be painful. Patients who experience pain with Plantar Fasciitis are suffering from inflammation and irritation of the plantar fascia. This the primary cause of pain and not the Heel Spur. Heel Spurs form in some patients who have plantar fasciitis, and tend to occur in patients who have had the problem for a prolonged period of time. While about 70 % of patients with plantar fasciitis have a heel spur, X-rays also show about 50 % of patients with no symptoms of plantar fasciitis also have a heel spur.
Diagnosis
Your doctor will discuss your medical history and will examine your foot and heel for any deformities and inflammation (swelling, redness, heat, pain). He/she will analyze your flexibility, stability, and gait (the way you walk). Occasionally an x-ray or blood tests (to rule out diseases or infections) may be requested.
Non Surgical Treatment
Perform some exercises. Exercises that strengthen and lengthen your plantar fascia can also be very helpful for heel spurs. Try some of the following activities. Calf stretch. Place your hands on a wall. Extend 1 foot (0.3 m) behind you with your knee straight and place the other foot in front of you with the knee bent. Push your hips toward the wall and hold the stretch for 10 seconds. You should feel a pull in your calf muscles. Repeat the stretch 20 times for each foot. Plantar fascia stretch, Perform this exercise in the morning before you've done any standing or walking. Cross your injured foot over the knee of your other leg. Grasp your toes and gently pull them toward you. If you can't reach your toes, then wrap a towel around them and pull on the towel. Hold the stretch for 10 seconds and repeat 20 times for each foot.
Surgical Treatment
Surgery to correct for heel spur syndrome is a common procedure which releases plantar fascia partially from its attachment to the calcaneous (heel bone). This part of the surgery is called a plantar fasciotomy due to the fact the fascia is cut. This is most often done through an open procedure as any heel spur or bursa can be removed at the same time. If the spur is not removed during the surgery, it will probably be just as successful, as the large spur is not the true problem. Some physicians use an endoscopic approach (EPF) where a small camera aids the physician during surgery with typically smaller incisions on each side of your foot.